NOW AVAILABLE AT BREACH CANDY HOSPITAL ON THURSDAYS 11:00 AM TILL 12:00 PM

Dr. Dilip Raja
Urologist & Andrologist
Prostate Cancer
practicing Urologist and Andrologist for more than 35 years
Get in touch with us today (022) 2645 2007
Prostate adenocarcinoma, Carcinoma of prostate, Cancer of prostate, Adenocarcinoma of prostate, Prostate carcinoma, Prostate malignancy, Prostate Tumour.
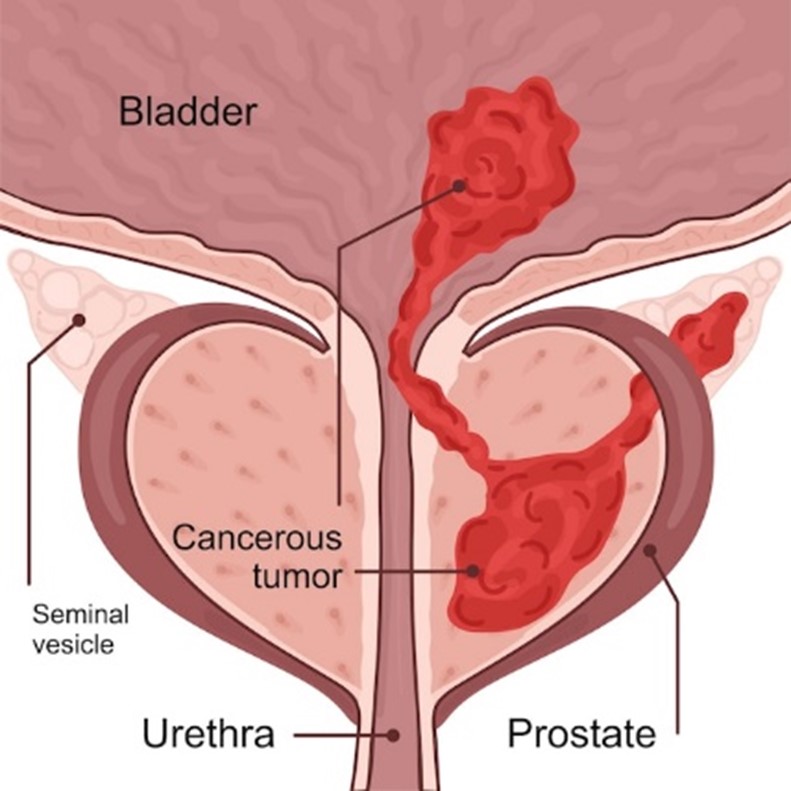
The prostate is a walnut-sized gland that forms part of the male reproductive system. The gland is made up of two lobes or regions enclosed by an outer layer of tissue. It is located in front of the rectum and just below the urinary bladder which is the storage organ for urine. The prostate gland surrounds the urethra, the canal through which urine passes out of the body.
The size of the gland varies with the age. In adult men, a typical prostate is about 3 cm thick and 4 cm wide and weighs about 20 grams. As the age advances, the prostate gland increases in size and can be anything between 40 grams to 100 grams or more.
Prostate cancer is one of the top ten leading cancers in India today. It usually affects men in the age group of 50+ years. However, recently there has been an increase in reports of cancer in younger men in the age group of 35-44 and 55- 64 residing in metropolitan cities.
Prostate Cancer, like any other cancer, develops from an abnormal growth and division of some cells leading to the formation of a tumour.
Prostate cancer can be more virulent or aggressive if found in younger individual. Older the age of a man slower is the growth of prostate hence, it is important to screen prostate regularly after the age of 50.
Causes Of Prostate cancer
- Old age
- Obesity
- Improper diet
- Genetic alterations have been identified as some of the main contributing factors towards an increased cause of prostate cancer
Risk Factors
There are four well-established risk factors for prostate cancer:
Men have a 1 in 6 lifetime risk of developing prostate cancer. It accounts to around 10000 deaths.
- Increasing age: -the older men get, the more likely a cancer might develop in the prostate.
- Ethnic origin: -Afro-Caribbean men are at higher risk than Caucasians and men from the Far East have a lower risk for cancer.
- Family history (genetic/heredity): -risk is increased if a father, brother or paternal uncle has prostate cancer.
- Obesity -Recent studies have shown that men who are overweight or obese are at significantly higher risk for developing prostate cancer.
However, there are some other factors which may impact risk of developing prostate cancer, which are not well understood.
However, early diagnosis and treatment could result in cure as early treatment of clinically significant prostate cancer has a very high cure rate.
Symptoms Of Prostate cancer
- Difficulty urinating,
- Hesitancy,
- Frequent urination
- Sense of incomplete voiding
- Taking a long time to pass urine
- Blood in the urine (haematuria).
These symptoms may or may not be present in early stage of prostate cancer. Hence, the regular screening is required. If the Prostate Cancer is detected and treated early the survival chances greatly increase. Please contact immediately your health provider best Urologist, Andrologist & Uro-Oncologist Dr. Dilip Raja Mumbai, India for complete treatment of prostate cancer.
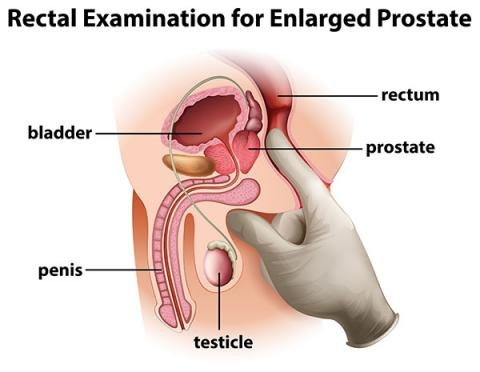
Physical Examinitation For Prostate cancer
The digital rectal exam (DRE)
Digital Rectal Examination by an experienced urologist is a must to differentiate between benign and cancerous prostate. A healthy prostate feels soft, rubbery, smooth, symmetrical, regular and even. Any lumps, or hard, woody or irregular areas of the prostate may indicate the presence of cancer and will require further testing.

Normal BPH

Tenderness

Symmetrical Enlarged

Asymmetrical

Induction

Nodularity
Investigations
- PSA TEST
- USG ABDOMEN & PELVIS WITH FULL BLADDER & POST VOID RESIDUAL URINE
- TRANSRECTAL ULTRASONOGRAPHY (TRUS) OF THE PROSTATE
- MRI OF PELVIS
- TRUS GUIDED PROSTATE NEEDLE BIOPSY
- BONE SCAN
- PET CT SCAN OR PSMA PET SCAN
- X-RAY CHEST PA VIEW
The PSA test

The most common prostate cancer test is the PSA, or prostate-specific antigen test. This is a simple blood test that measures the presence of prostate-specific antigen, or PSA, circulating in your bloodstream. This test is usually the first step in any prostate cancer diagnosis. The PSA test is also used to track the effects of prostate cancer treatment such as surgery, radiation, hormone therapy and chemotherapy.
Readings -Cancer detection
PSA levels
- Normal – 0 TO 4 ng/dl
- Borderline – 4 – 10 ng/dl
- Significant –more than 10 ng/dl
Once DRE and PSA are suspicious of prostate cancer, the next step is to do USG of abdomen and pelvis with post void residual urine subsequently, MRI of the prostate before doing Prostate Biopsy.
USG For Abdomen & Pelvis With Full Bladder And Post Void Residual Urine Combined With Transrectal Ultrasonography (TRUS) Of The Prostate
- The urinary system and also measure the status of both kidneys.
- Bladder Capacity and Post Void Residual Urine.
- Approximate size of the Prostate Gland.
MRI of The Pelvis(Magnetic Resonance Imaging)
MRI of the pelvis will not only detect the irregularity of prostate but also give an idea of local extension of the prostate cancer, if present. MRI will also give us a clue of the prostate spreading outside capsule of the prostate or into the lymph nodes.
Guided Prostate Biopsy
The TRUS guided prostate needle biopsy is done under local anaesthesia in a sonography unit. Trans rectal ultrasound guided biopsy of prostate is used to take 12 – 16 cores of prostatic tissue through a needle inserted into the rectum under ultrasound guidance. The tissues are taken and sent for histopathology examination.
Bone Scan
After a bone is damaged by tumour, new bone tissues grow. A bone scan can detect this new growth may show that cancer has spread into the bone. Bone scan is done to see for the spread of the cancer to the bone.
PET CT Scan Or PSMA PET Scan
PSMA Pet Scan is an imaging test use to detect prostate cancer throughout the body. It uses a radioactive substance that targets protein called PSMA, or Prostate Specific Membrane Antigen which is expressed by the Prostate Cancer.
X RAY CHEST PA VIEW
Grading of Prostate cancer
- The pathologist grade cancer cell removed during biopsies
- Low grade looks more like normal cells
- High grade, cell may vary in size and shape
- Cell from two biopsy site is graded using Gleason score of between 2 –10. The higher the score, the more likely cancer cells will grow faster and spread. The pathologist will give your doctor a report about biopsy.
Gleason’s Score
The Gleason’s score not only keeps grades the disease but also predict the prognosis of prostate cancer.
| Score 0 – 6 | Score of 7 | Score up to 8 – 10 |
| The cancer could be slow growing tumour and many a times a conservative approach may be taken and if the cancer is small and localised, prostate cancer patient can be kept under wait and watch policy and the prostate cancer may not be virulent and may not require any further treatment. | This kind of prostate cancer grows and spreads and it is important to treat rather than wait and watch. | The cancer is likely to grow and spread fast and may have already spread to other organs. The disease can be quite aggressive and further evaluation may be necessary to check on the spread of the cancer called metastasis. |
Stages Of Prostate cancer
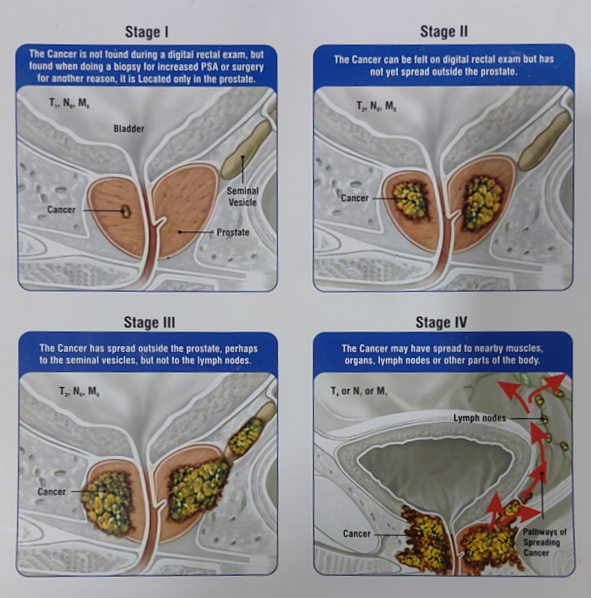
The staging of prostate cane is determined by the knowledge of spread of the cancer. It can be localised or locally & distantly spread. The following diagram will aptly describe the staging of the prostate cancer.
- Stage I – Cancer is considered slow growing, and the tumour can’t be felt during Digital Rectal examination and involves one-half of one side or less of the prostate.
The cancer cells look similar to healthy cells, and the PSA levels are low. - Stage II – Cancer is found only in the prostate and can be felt during the digital rectal examination of prostate. While the tumour itself is small, it has a higher risk of growing or spreading to other areas of the body.
PSA levels are low or medium.
- Stage III – High PSA levels, the tumour shows signs of growth outside of prostate perhaps to the seminal vesicles but not to the lymph nodes, or the cancer is considered high grade.
- All of these factors may indicate that the cancer could grow and spread.
- Stage IV – The cancer has spread beyond the prostate to other areas of the body to the nearby muscles & lymph nodes.
Treatments Of Prostate cancer
Various treatment options are employed:
- Active Surveillance
- Radical Surgery
- Radiation therapy
- Hormonal therapy
- Chemotherapy
Active Surveillance
Active surveillance is recommended if the prostate cancer is small and of low grade. During the surveillance the patient is asked to do repeat PSA test at variable intervals along with DRE examinations. Sometimes repeat biopsy may require.
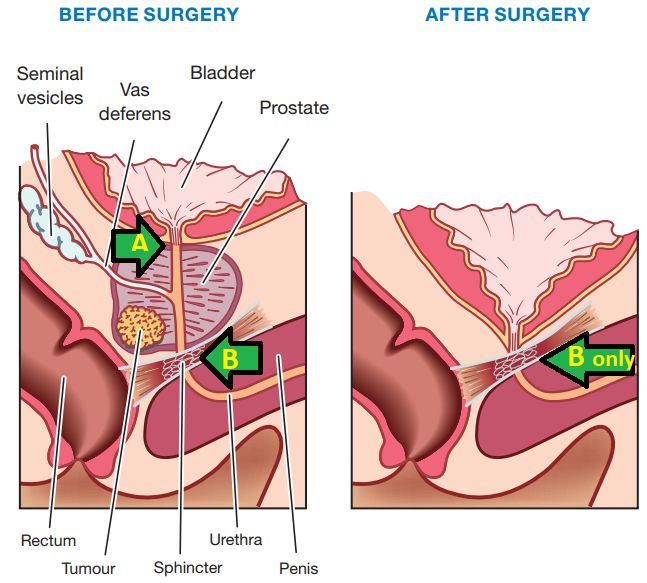
Radical Prostatectomy
This is a surgical removal of prostate gland primary to remove entire growth of prostate cancer along with Seminal Vesicle. This surgery can be performed if the prostate cancer is limited and restricted to prostate gland and part of urethra & has not spread outside the gland. If necessary, a pelvic lymphadenectomy is performed to remove nearby pelvic lymph nodes.
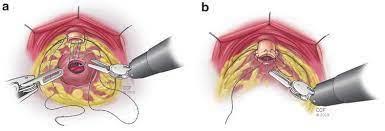
This can be achieved by :
- Open Radical Prostatectomy
- Laparoscopic Radical Prostatectomy or
- Robotic Radical assisted Prostatectomy (RARP)

Radiation Therapy – External beam
This therapy gives radiation to the localised area to kill the prostate cancer cells. This is generally undertaken if the surgery is too risky because of their medical conditions like history of cerebral stroke, coronary bypass (CABG), poor general health of patient or any other contra indications. Generally, radiation therapy takes more than 30 – 35 sessions and treatment spread over period of 03 months. This can be undertaken as primary therapy is selected cases.
Radiation therapy – Brachytherapy
Low-dose seed implant brachytherapy
The seeds are inserted through the skin in the perineum (the area between the anus and scrotum). Procedure is performed under either general or spinal anaesthesia and lasts approximately 1 hour.
High Dose Brachytherapy (HDR)
Under anaesthesia, approximately 15 needles are inserted through the perineum. These needles are wired to the radiation source that delivers a high radiation dose to the prostate. The needles are then removed. The treatment takes 10–20 minutes.
Treatments Of Advance Prostate cancer
- Hormone therapy
This therapy is generally used if prostate cancer has spread outside of the prostate gland or recurrence of prostate cancer after any other mode of therapy used in the past. This can be done by either medical or surgical orchidectomy.
- Bilateral Subcapsular Orchidectomy
Bilateral subcapsular orchidectomy is performed to remove the substance of the testicles which in turn stimulates growth of the prostate cancer cells. This is called surgical orchidectomy. Once again if the surgery is contradictory, medical orchidectomy can be done.
- Chemotherapy
Further, the Specific Anti-Cancer Drugs are used in advanced, metastatic or recurrent cancer where even hormone therapy also failed.
Follow-Up Treatments
- Follow up care to be discussed with your Uro-Surgeon
- Every treatment of prostate cancer may have some side effects and complications related to the treatment options. This needs to be understood and accordingly counselling and /or prevention therapy will be advised by you Uro-Onco surgeon Dr. Dilip Raja, Bandra west, Mumbai.
- Good Nutrition – to be discussed after completion of successful treatment.
Preventions
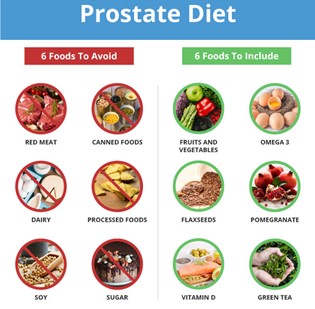
- Some risk factors –such asrace, – family history or age -cannot be modified, while others, especially diet and weight, can be controlled.The Prostate Cancer Foundation suggests that men wanting to reduce their risk of prostate cancer.
- Eat fewer red meats and high-fat dairy products
- Good Nutrition – to be discussed after completion of successful treatment.
- Eat five or more servings of vegetables and fruits each day,
- Exercise regularly and
- Maintain a normal weight.